Table of Contents
ToggleSedation Dentistry: Easing the Fear of the Chair
You aren’t alone if the thought of a dental chair makes your heart race for Sedation Dentistry. I used to dread even routine cleanings. But discovering the gentle power of Sedation Dentistry changed that — for me, for a friend, maybe it could for you too. Below, I share what I learned (with a few bumps, a bit of skepticism, and eventual relief). It isn’t a dry medical manual — it’s a candid, human take on calming dental anxiety and getting the care you need without holding your breath in dread.
What Exactly Is Sedation Dentistry?
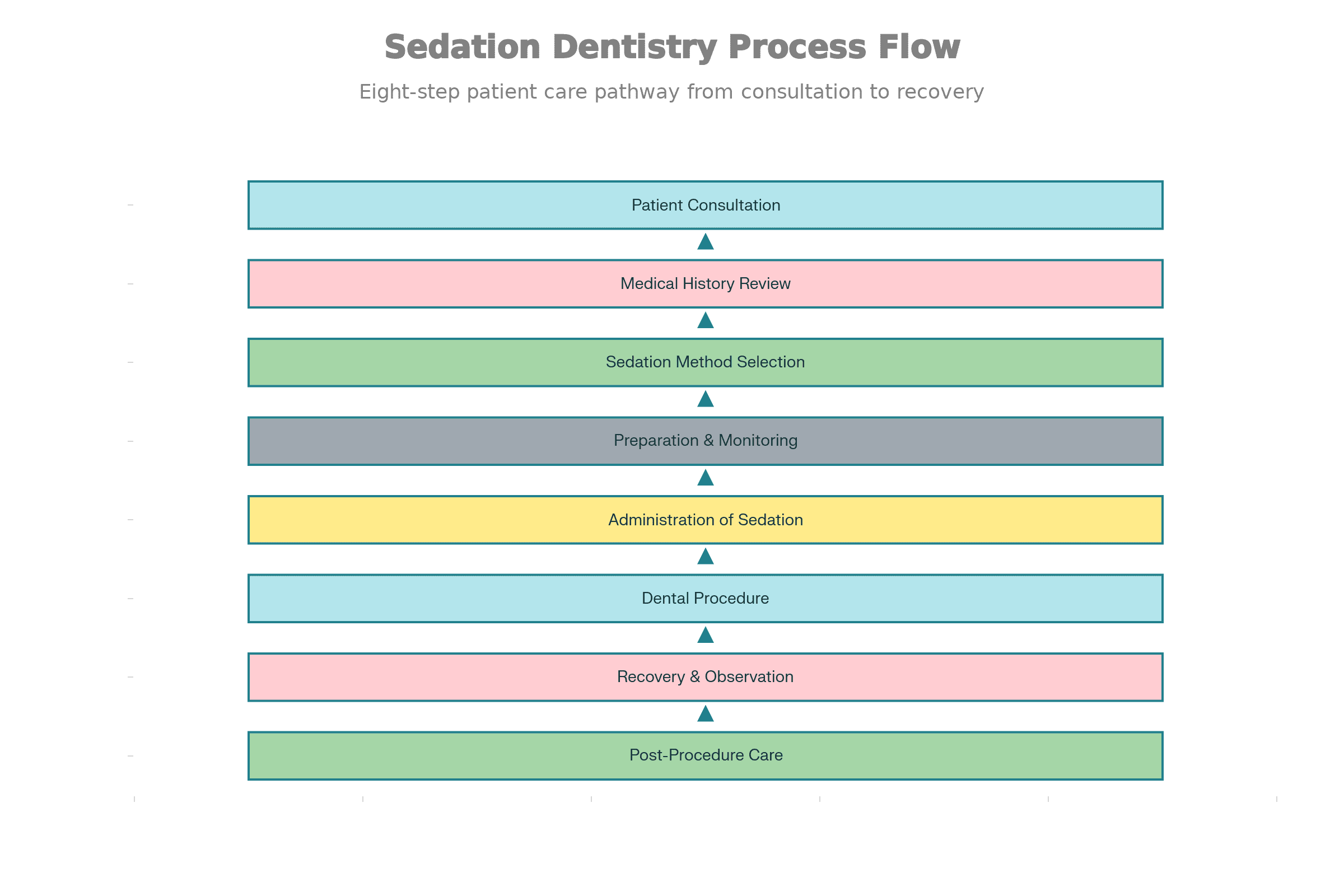
So what do we mean by “sedation dentistry”? Simply put: it’s using medication to ease anxiety (and sometimes awareness) during dental procedures. The term covers a range of approaches — from a mild calming effect to a deeper sedation — depending on what you and your dentist decide. According to the trusted definition, sedation can range from minimal relaxation to deep sedation (though deep sedation and general anesthesia are different beasts).
Common methods include inhaling nitrous oxide (the so-called “laughing gas”), taking an oral sedative about an hour before your visit, or — for more involved procedures or severe anxiety — intravenous (IV) sedation directly into the bloodstream.
Why the Range from Mild to Deep?
Each patient is unique. Some may only need a gentle calming — maybe they hate needles or have a sensitive gag reflex. Others might face real dental phobia, need a long procedure, or struggle with staying still (kids or people with sensory sensitivities come to mind). Sedation dentistry offers a flexible “slider” of comfort: minimal, moderate, deep — whichever level helps you sit still without panic.
How Sedation Dentistry Helped — My Story (and a Friend’s)
I’ll be blunt: I avoided the dentist for years. Cleanings, fillings — I pushed them off because of what I’d heard (pain!) or feared (the drill, the chair, the unknown). Then one day, after a particularly persistent toothache, I swallowed my pride and booked a consult. The hygienist asked whether I was comfortable with sedation, and I said yes, thinking, “Better safe than sorry.”
The nitrous oxide mask went on. Within minutes, I felt calm — somewhat lightheaded. The usual flutter of nerves vanished. The cleaning was done before I even fully registered it. I remember thinking, “Is that it?” In hindsight: yes — that was it. A quick, anxiety-free visit. I drove home, had my coffee, and all felt normal. No fuzziness, just relief.
Later, a friend needed a root canal — major for her, emotionally and physically. She opted for oral sedation + local numbness. She told me afterward, “I woke up, and it was over. I couldn’t tell you if they drilled or filled or did whatever.” No trauma, no flashbacks. Just clean teeth and a grateful grin.
Would either of us have had that kind of ease without sedation? I doubt it. And that — to me — makes sedation dentistry more than a procedure. It’s liberation from dental fear.
When Sedation Dentistry Makes Sense — and When It’s Overkill
Not everyone needs sedation — but for many, it drastically improves dental care access. Here’s a rough breakdown of who tends to benefit:
- People with dental anxiety or phobia (afraid of drills, needles, gag reflex, or even just the chair itself).
- Patients needing longer or complex procedures (root canals, major fillings, extractions, multiple crowns).
- Those with a sensitive gag reflex or difficulty being numbed with just local anesthesia.
- Individuals with special needs, sensory sensitivities, or conditions that make staying still difficult.
- Anyone who simply doesn’t want to dread their dental appointment every time, even routine cleanings, can feel easier with minimal sedation.
On the flip side, sedation might be overkill for a simple check‑up and cleaning if you have no anxiety. Every intervention has potential side effects (drowsiness, dry mouth, maybe nausea), and for stronger sedation, you’ll need someone to take you home.
Risks, Safety & What Your Dentist Should Do — Because You Deserve Transparency
Yes — sedation dentistry is widely helpful. But it isn’t magic. Like any medical intervention, it comes with caveats.
Potential side‑effects include drowsiness (lasting hours), dry mouth, perhaps a mild headache or nausea after, especially with oral or IV sedation. For those receiving IV sedation or stronger medication: you shouldn’t drive home; you’ll need a companion.
In rare cases, if sedation isn’t handled properly — or the patient has underlying conditions — there can be risks to breathing or cardiovascular functions. That’s why sedation should only be administered by trained professionals, with proper monitoring (heart rate, blood pressure) during the procedure.
Also — sedation ≠ pain relief. Dentists still rely on local anesthetics to block pain. Sedation helps with anxiety and memory, but numbing ensures you don’t feel drilling deep inside your jaw.
Bottom line: sedation dentistry gives a margin of safety and comfort — but it’s important to have an honest pre‑procedure evaluation. Disclose allergies, medications, your overall health. Ask what sedation level is being offered, what drug will be used, and how long recovery typically lasts.
—
What to Ask Before You Say “Yes” to Sedation
Here’s a little “checklist” I wish I had before my first sedation‑aided visit. Maybe it helps you too:
- Which type of sedation will I receive? (Nitrous oxide / oral pill / IV?)
- How long before the procedure should I stop eating or drinking?
- Will I need someone to accompany me afterward — to take me home?
- What are the expected side effects, and how long will they last?
- If I feel anxious but otherwise healthy, do I really need deep sedation — or will minimal/moderate do?
- What local anesthesia will be used? Sedation doesn’t guarantee pain‑free without numbing.
- What happens if I have allergies or prior reactions to sedatives? Is there an alternative?
It’s okay (and smart) to ask these. You’re paying attention to your health — not being “difficult.”
—
Can Sedation Dentistry Help Overcome Dental Fear Over the Long Haul?
Here’s a thought: sedation isn’t just a “band‑aid” for dental anxiety. For many, it’s a bridge — a way back into a normal care routine after years (or decades) of avoidance. I know a friend who literally skipped cleanings for over five years out of fear. After sedation‑assisted treatment, she went back to routine check‑ups without a second thought.
In behavioral dentistry literature, treatments like sedation — combined with gentle communication, calming environment, and trust-building — are often more effective than just numbing pain. They may help reshape a patient’s attitude to dental care overall.
Think of it like training wheels: once you ride confidently, you may never need the sedation again — but it got you started, and helped you stay on track.
My Lessons Learned (And What I’d Tell My Past Self)
- You deserve comfort and dignity.** Dental fear is real — and you don’t have to “tough it out.” Sedation dentistry offers real empathy, not just a drill and mask.**
- Minimal methods like nitrous oxide can make even regular cleanings painless and anxiety‑free. It doesn’t have to be a “big deal.”
- If you’ve been avoiding dental care for years because of fear, sedation might be the reset button. Don’t let fear rob you of oral health (or confidence!).
- But always stay informed. Understand what sedation really means (not “being knocked out”). Ask questions. Advocate for yourself. You own your body, and you deserve clarity and respect.
—
Looking Forward — Is Sedation Dentistry Becoming the Norm?
Given increasing awareness around dental phobia, mental health, and overall dentistry experience, I believe sedation dentistry is slowly but surely becoming more accepted — not just as a “luxury” but as a legitimate standard, especially for anxious patients or complex procedures. More clinics are offering it, more dentists are trained, and patients are speaking up: they want comfort, not pain. That’s a shift worth cheering.
If you want to explore reputable clinics or get a sense of sedation‑ready practices, you might start with trusted resources and directories — like this dental‑care directory, because the right care shouldn’t be hard to find or scary to ask for.
Final Thoughts — The Chair Doesn’t Have to Be a Source of Fear
Fear of the dentist isn’t silly. It’s real. And if that fear keeps you from necessary care, then sedation dentistry can be a tool, a comfort, a reprieve. Remember: it’s not about “bravery,” it’s about care. If calming meds help you sit back and let healing happen — that’s smart, not weak.
So if you’ve avoided the dentist for years, or you shake just thinking of the needle, maybe give sedation dentistry a chance. Ask questions. Seek a certified dentist. Bring a friend for support — and for a ride home. You might leave with a healthier smile… and a lighter heart.